SHORT REPORT
Is a stable positive rate of <0.1% an indication of a fresh outbreak of SARS-CoV-2 infection?
Alberto Boretti*
Deanship of Research, Prince Mohammad Bin Fahd University, Al Khobar, Saudi Arabia
Abstract
This letter gives a short analysis of the rate of positive SARS-CoV-2 tests in New Zealand and the restrictions that were implemented in response to these rates changing. Concerned about the growth of the number of positive cases of SARS-CoV-2 infection, the New Zealand government introduced stricter lockdown measures on August 16, 2020, and on August 18, 2020, it postponed elections planned for September. Growth in the number of positive cases was an artifact of the number of tests growing at a higher rate than the number of positive cases. The positive rate on August 16 was 0.05% (13 positive cases from 26,014 tests). On August 2, the positive rate was higher at 0.18% (three positive cases from 1,692 tests), despite the government considering that the virus was eradicated at this time. A better approach to this pandemic would be the development of policies based on the positive rate, not solely on positive case numbers, and to include viral load using reverse transcription polymerase chain reaction (RT-PCR) tests with an appropriate cycle threshold to properly identify infectious cases. It is also advised to protect vulnerable populations and avoid unnecessary limitations to the healthy population. The SARS-CoV-2 pandemic will last longer than several months, and the sooner life gets back to nearly normal, the better.
Keywords: COVID-19; coronavirus; incidence rate; lockdown; pandemic; New Zealand
Citation: Int J Infect Control 2021, 17: 20927 – http://dx.doi.org/10.3396/ijic.v17.20927
Copyright: © 2021 Alberto Boretti. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 5 June 2020; Revised: 17 September 2020; Accepted: 18 December 2020; Published: 24 September 2021
Competing interests and funding: The author received no funds and has no conflict of interest to declare.
*Alberto Boretti, P.O. Box 1664, Al Khobar 31952, Kingdom of Saudi Arabia. Email: a.a.boretti@gmail.com
The management of the SARS-CoV-2 infection has been characterized by significant differences around the world, with often worse epidemiological outcomes in countries that adopted harsher restrictions versus countries that adopted more sustainable measures (see the case of Belgium and the United Kingdom versus the case of the Netherlands or Sweden). Here, we discuss the full lockdown implemented in New Zealand as the result of questionable epidemiology based on tiny numbers of increased positive cases while neglecting the much larger number of tests performed to measure these positive cases. Going in and out of lockdown is not sustainable and only damages the economy and society without resolving the underlying issue. This has now been acknowledged by the vast majority of independent scientists, as clearly indicated by the success of the Great Barrington declaration gbdeclaration.org, despite the ostracism by media, with the World Health Organization calling for world leaders to stop locking down their countries and economies.
On August 16, in fear of growing case numbers of SARS-CoV-2 infection, the government of New Zealand introduced harsher restrictions for the Auckland region (1), and on August 18, 2020, the elections planned for September were postponed (2). This response was dramatic, based on the artifact of growing case numbers proportional to the similarly growing number of tests within the context of a perfectly stable, negligible, and positive ratio.
Charts in Fig. 1 show the number of new cases, the number of new tests and their ratio, and the positive ratio for New Zealand plus a map of the positive ratio across the world as measured today (Fig. 2). At peak outbreaks in western Europe, the positivity ratio was much higher. In the United Kingdom, for example, it was above 30% on April 10. While very high positivity rates are an indication of testing limited to the sickest patients missing mild or asymptomatic cases, lower positivity rates that indicate inclusion in the testing of patients with mild or asymptomatic should remain at 5% or slightly lower for at least 14 days in the presence of a SARS-CoV-2 outbreak. In New Zealand, the positivity ratio peaked at 3.9% on March 31, at roughly one-tenth of the values in the United Kingdom, and at the time of writing, it was stable at <0.1% since April 30, following only minimal oscillations. The asterisk close to the positivity rate indicates a value computed as the ratio of daily new cases to daily new tests. The positivity rate proposed by ourworldindata.org is computed differently through smoothing. As it may take 1–3 days to get the result of a test, the new cases reported on a specific day are the result of tests performed 1–3 days before.
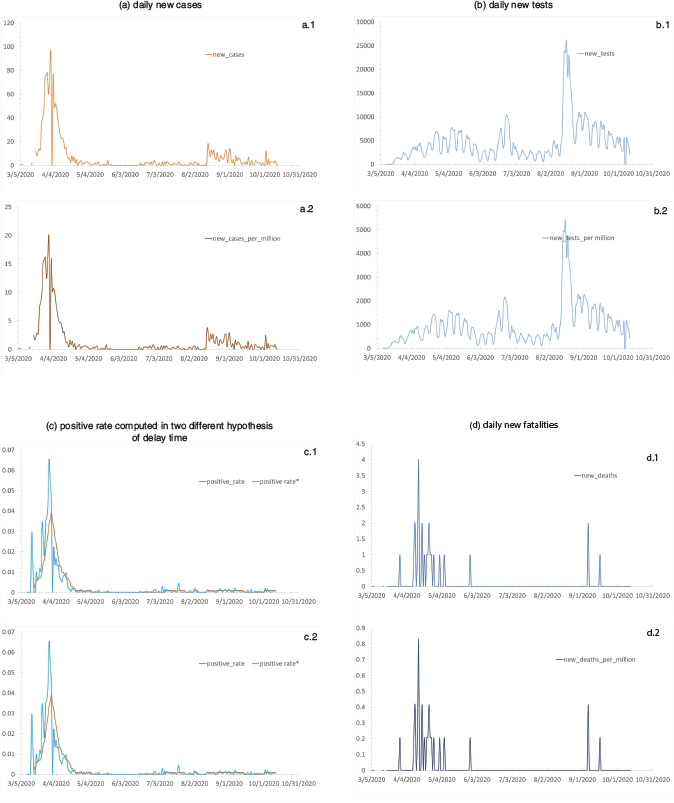
Fig. 1. (a–d) SARS-CoV-2 new cases, new tests and their ratio, the positive rate, and new deaths for New Zealand (NZ). Updated to October 12, 2020. The NZ positivity rate is one of the world’s lowest, and it did not change from the time SARS-CoV-2 was declared as eradicated to the time a dangerous second wave was declared. Data and images from Max Roser, Hannah Ritchie, Esteban Ortiz-Ospina, and Joe Hasell (2020) – ‘Coronavirus Pandemic (COVID-19)’. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/coronavirus’ [Online Resource]. Accessed October 13, 2020.
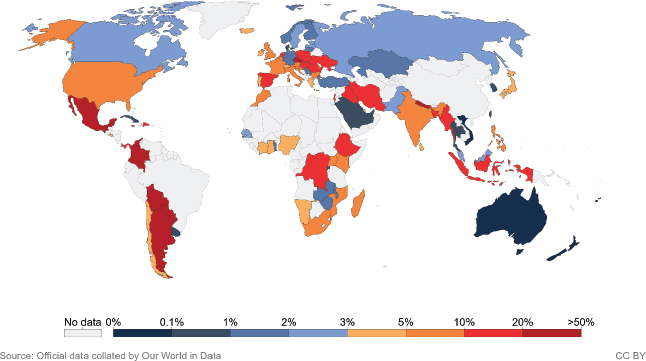
Fig. 2. Map of the latest positivity rate across the world. Updated to October 12, 2020. New Zealand and Australia have the world’s lowest cases.
The number of positive cases was <0.1% for many months. However, minimal background infectivity due to coronaviruses is always detectable when performing a significant number of tests. It does not make any sense to measure even higher than usual percentages of infected-over-tested and declare New Zealand as SARS-CoV-2 free. For example, on August 2, there were three positive cases from 1,692 tests, a positive rate of 0.18%, and a declaration that SARS-CoV-2 had been fully eradicated – which is perhaps impossible. However, there were 13 positive cases from 26,014 tests on August 16, which were proof of a ‘fresh outbreak’ when the positive rate was less at a tiny, insignificant 0.05%.
The RT-PCR test for SARS-CoV-2 has well-known limitations. It is currently based on many amplification cycles that are excessive (3–7). As the cycle number for positivity is usually omitted from the result, it is only a qualitative assessment not returning any viral load, making no distinction between patients with live viruses and patients with only viral fragments (3–8). The test amplifies in cycles minuscule amounts of DNA material to make an amount large enough to be detected. By adopting an excessive number of amplification cycles, patients with only a tiny amount of viral fragments can also be declared positive. The cycle threshold (CT) of 40 is recognized as excessive. In the sets of testing data that include CTs from three states of the United States (US), up to 90% of the positive carried hardly any virus (8). Any test with a CT above 35 is definitively too sensitive (3, 4). The US Centers for Disease Control and Prevention (CDC) states that a threshold of 33 cycles would be more appropriate. A more reasonable cutoff could be even less, at approximately 30 (4). If a CT of 30 is used instead of the current 40, as a ~3.3 increase in the CT value reflects a 10 times reduction in starting material (4), 1,000 times larger amounts of viral material in the sample would be needed for positivity. Mass testing for SARS-CoV-2 viral fragments with RT-PCR tests with CT of 40 will return some positive results at positive rates of 0.05 to 0.10% for a very long time.
The latest restrictive measures and postponing of elections in New Zealand appear to be an over-reaction not supported by epidemiological logic. While the way out of this pandemic remains uncertain worldwide, without a doubt, any restrictive measures should be based on sound epidemiological parameters. As mentioned by ourworldindata.org – but ignored in New Zealand – ‘it is not informative to look at case counts in isolation’ because ‘without testing, there is no data’.
The majority of institutions, from Johns Hopkins University (https://coronavirus.jhu.edu/) and the CDC (http://www.cdc.gov), reports the total daily number of positive test results as a percentage of the number of tests performed that day; this is because the percentage of laboratory tests positive for SARS-CoV-2 is the most important parameter for understanding the evolution of the outbreak. For some reason, New Zealand considered a very singular metric to enforce more severe restrictions and postpone elections.
In New Zealand, there had been to date 1,872 coronavirus cases and only 25 deaths. The 1,802 recovered cases left the number of open cases at 45. To put it into perspective, more than 200,000 people contract the flu each year in New Zealand, and many of them die either directly or indirectly from its effects. According to the Ministry of Health (https://www.health.govt.nz/publication/mortality-2016-data-tables), in 2016 (the last year on record), 1,740 people died of chronic lower respiratory diseases, and 711 people died of influenza and pneumonia.
Complete lockdowns that go up and down for more than 5 months with the cancellation of general elections are not a reasonable response to SARS-CoV-2 infection based on epidemiological evidence. The case of New Zealand calls for objective rather than subjective criteria to determine the severity of an outbreak and to design appropriate measures that could permit the safety of the vulnerable and societal sustainability.
The way to move forward in the COVID-19 pandemic is not to limit infection through harsh restrictions that fluctuate in response to changing positive case numbers. Such restriction measures are not sustainable (9, 10). They put a country at risk of second waves, real or fictitious. Restoring harsh measures brings the economy and society to a stand-still (9, 10), adding further damage. More carefully designed measures should be based on epidemiological data, that is, the positive rate, rather than the absolute number of positive cases. Such measures should be sustainable, avoiding unnecessary limitations to healthy populations that have limited risk of serious consequences from the SARS-CoV-2 infection, while protecting the vulnerable and offering effective hospital care for those in urgent need (9, 10).
Restrictions should not be based on the number of new cases in isolation, even if this practice is followed by many jurisdictions, such as Victoria, Australia (11), which has used the same approach as New Zealand. Viral load is another parameter presently missing in policing SARS-CoV-2. The currently adopted RT-PCR test uses an excessive CT of 40, which recognizes as positive those cases with only viral fragments that represent very little infectivity (3). A better approach to this pandemic could be designed by also using the positive rate, as advocated in this paper, and by more properly detecting infectious cases. Positive results detected after more than 35 cycles of exponential growth should be definitively neglected, and those with RT-PCR test results of 30–35 should be simply directed to further examination rather than being declared infectious (3).
The development of policies based on positive rate, not on positive case numbers, including viral load would be a better approach to this pandemic. It is also advised to protect the vulnerable population and avoid unnecessary limitations to the healthy population. The SARS-CoV-2 pandemic will last longer than a few months, and the sooner life gets back to nearly normal, the better. The message from the Great Barrington declaration is clear.
Disclaimer
The opinions and views expressed in this paper are solely those of the author.
References
- Hollingsworth J. CNN New Zealand imposes 12-day lockdown in its biggest city as it battles fresh outbreak. 2020. Available from: edition.cnn.com/2020/08/14/asia/new-zealand-coronavirus-lockdown-intl-hnk/index.html [cited 12 October 2020].
- Cullinane S, Beech S. New Zealand Prime Minister Jacinda Ardern delays election over Covid-19. 2020. Available from: edition.cnn.com/2020/08/16/asia/new-zealand-ardern-election-delay-coronavirus/index.html [cited 12 October 2020].
- Boretti A. Cycle threshold as a measure of infectivity from Covid-19 PCR tests. Afr J Respir Med 2020; 15(1): 13–15.
- Tom MR, Mina MJ. To interpret the SARS-CoV-2 test, consider the cycle threshold value. Clin Infect Dis 2020; 71(16): 2252–4. doi: 10.1093/cid/ciaa619
- Joynt GM, Wu WK. Understanding COVID-19: what does viral RNA load really mean? Lancet Infect Dis. 2020; 20(6): 635–6. doi: 10.1016/S1473-3099(20)30237-1
- Geddes L. Puzzle over viral load. New Sci 2020; 245(3276): 8. doi: 10.1016/S0262-4079(20)30658-8
- Jefferson T, Heneghan C. COVID-19: clinical utility of cycle threshold values. 2020. Available from: www.cebm.net/study/covid-19-clinical-utility-of-cycle-threshold-values/ [cited 12 October 2020].
- Mandavilli A. Your coronavirus test is positive. Maybe it shouldn’t be. 2020. Available from: www.nytimes.com/2020/08/29/health/coronavirus-testing.html [cited 12 October 2020].
- Boretti A. After less than 2 months, the simulations that drove the world to strict lockdown appear to be wrong, the same of the policies they generated. Health Serv Res Manag Epidemiol 2020; 7: 1–11. doi: 10.1177/2333392820932324
- Boretti A. Sustainable post Covid19 lockdown strategy through evidence-based policy: analysis of Covid19 fatalities across Europe. Integr J Med Sci 2020; 7: 172. doi: 10.15342/ijms.7.172
- Boretti A. Covid19 outbreak in Victoria, Australia update August 1, 2020. Health Serv Res Manag Epidemiol 2020. doi: 10.1177/2333392820960350